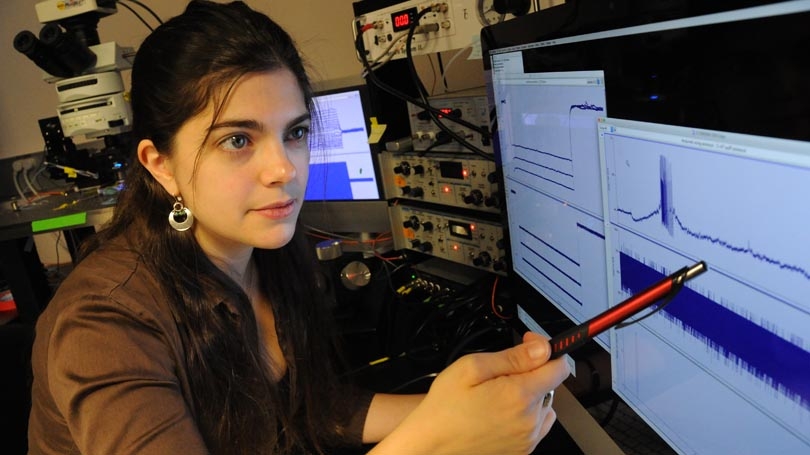
Emily Stephens in the Borwell Research Laboratory at Dartmouth Hitchcock Medical Center.
Depression, which affects approximately 8% of Americans over the age of 12, is a prevalent psychiatric disorder characterized by tiredness, sadness, lack of interest in daily activities, reduced concentration, reckless behaviors, and in some extreme cases, suicidal ideation.
In many cases, depression involves the disruption of signaling of a neurotransmitter called serotonin (5-hydroxytryptamine, 5-HT), which is made by neurons in the brainstem, but released throughout most areas of the brain. Drugs that alter serotonergic transmission are commonly prescribed to millions of patients for treatment of depression, anxiety, and other mood disorders.
These drugs, called selective serotonin reuptake-inhibitors (SSRIs), are currently prescribed to 1 in 10 Americans with an even larger population of women between the ages of 40 and 59 years taking these drugs (23%). The primary effect of SSRIs is to increase the amount of 5-HT in the brain, facilitating serotonergic functioning. However, increasing 5-HT levels in the brain is not itself sufficient to ameliorate symptoms of depression, as these drugs often take weeks to improve mood in patients, suggesting that an additional, slowly developing change is responsible for the therapeutic efficacy of SSRIs. An important question facing neuroscience today is, what is the neurological mechanism underlying the therapeutic efficacy of SSRIs?
I am interested in how 5-HT affects neurons of the prefrontal cortex (PFC), an area of the brain centrally involved with depression. The PFC is located in the frontmost part of the brain and controls impulses and emotions, regulates behaviors, and is otherwise involved with executive functioning. Importantly, patients diagnosed with depression are often found to have deficits in executive functions such as planning and short-term memory.
In my previous work researching 5-HT in the PFC, I have found that the physiological responses to 5-HT of different cortical neurons vary based on differences in expression of 5-HT receptors, which are proteins located on neurons that detect 5-HT in the brain. In addition, these differences in 5-HT responsivity are based on what area of the brain the neuron in question is communicating with.
Neurons in the PFC communicate with other areas in the brain via long-range connections, called axons, similar to electrical wires. In order to identify populations of cells based on where their axons communicate, I can inject a substance called a retrograde tracer into a single area of the brain. These retrograde tracers will be absorbed by the axons in the injected area and transported back to the main body of the cell. After this happens, I am able to see these retrograde tracers inside single neurons in the PFC that send an axon to my injection location and easily target those cells for testing. These tools allowed me to test my hypothesis that chronic SSRI treatment would change the expression pattern of 5-HT receptors in one population of PFC neurons that send axons to specific places in the brain, resulting in a change in 5-HT responses in that population of cells.
For my experiments, I injected retrograde tracers into the brainstem to label cells sending axons to an area called the pons. I injected this tracer into the brain of a rat that received the most commonly prescribed SSRI, fluoxetine (Prozac), via osmotic pump, continually for three weeks. These osmotic pumps are implanted beneath the skin and slowly deliver a specific amount of fluoxetine to the rats.
After this treatment and injection, I measured 5-HT responses in the population of cortical neurons that were labeled with retrograde tracers (cells sending axons to the pons). I found that after three-weeks of treatment with an SSRI, inhibitory 5-HT responses increased in my labeled population of cortical neurons. Importantly, this same population of neurons responded to 5-HT with an excitatory response in control animals.
This finding was very exciting as an almost complete switch from excitatory to inhibitory 5-HT responses was recorded in the rats I tested. This data is important as increased inhibitory signaling in the PFC may play a role in decreasing depressive behaviors and may serve as a potential substrate underlying the delayed action of long-term SSRI use. I plan to continue my research on this project by testing the behavioral changes that occur in these rats with long-term treatment of SSRIs.